o It is 10-15% common. It is common in females.
o It can occur either de nova or in a pre-existing multinodular goitre.
o Thyroglobulin immunostaining is positive.
Types
a. Noninvasive-blood spread not common.
b. Invasive-blood spread common.
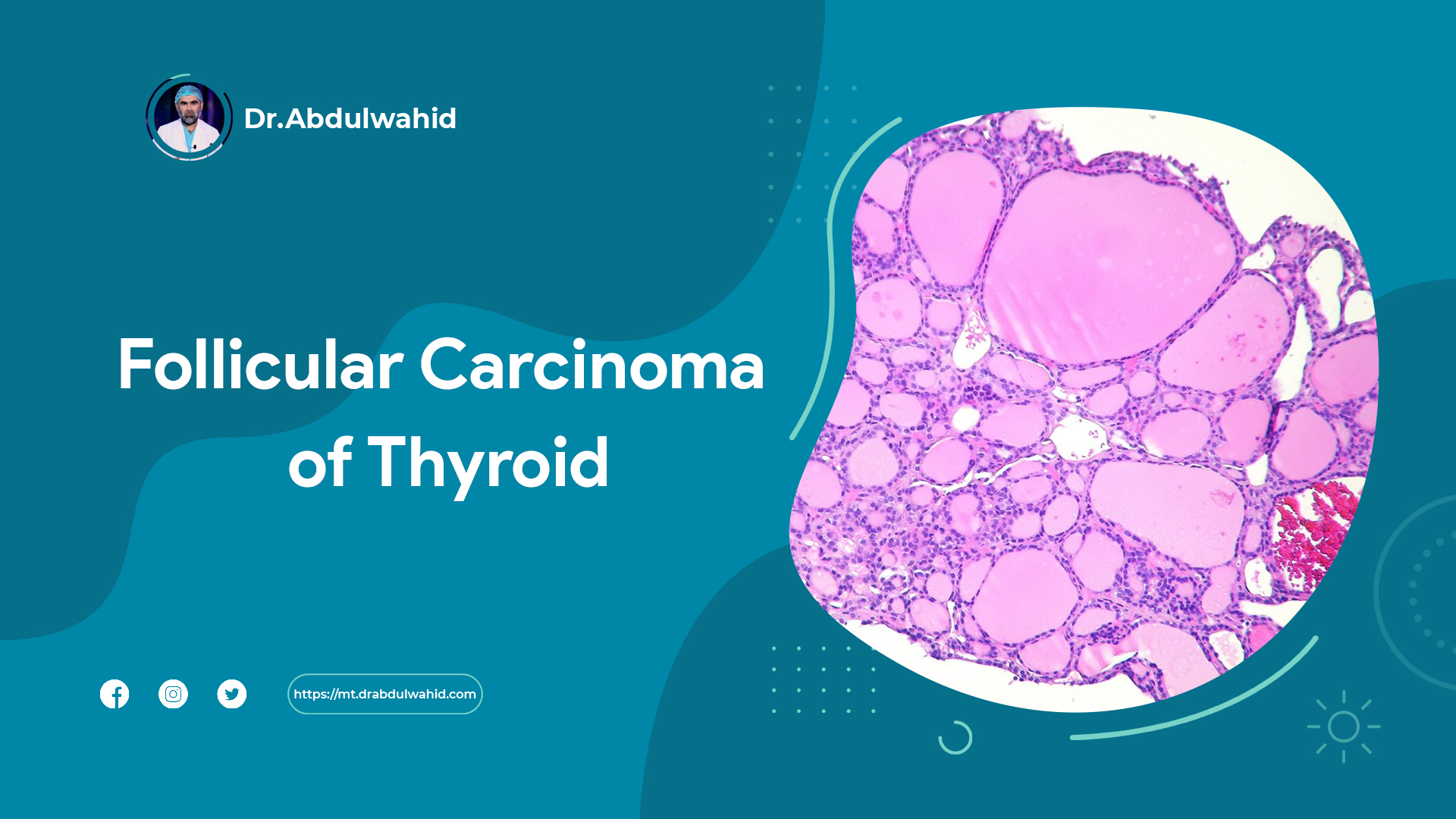
Typical features: Capsular invasion and angioinvasion.
Spread
It is a more aggressive tumour.
It spreads mainly through blood into the bones, lungs, liver. Bone secondariesare commonly seen in skull (frontal bone), long bones and ribs; in the skull, it is typically warm, vascular, localized, nonmobile and pulsatile. As both outer and inner tables of the skull is disrupted and since it is OTC metastases it contains colloid; so brain pulsation is transmitted to scalp across the disrupted skull tables through fluid colloid.
It can also spread to lymph nodes in the neck occasionally (10%) .
Clinical Features
o Swelling in the neck, firm or hard and nodular.
o Tracheal compression/infiltration and stridor.
o Dyspnoea, haemoptysis, chest pain when there are lung secondaries.
o Recurrent laryngeal nerve involvement causes hoarseness of voice, +ve 'Berry's sign' signifies advanced malignancy (infiltration into the carotid sheath and so absence of carotid pu lsation) .
o Well localised, nonmobile, soft, fluctuant (because of colloid content) and pulsatile (as both inner and outer tables of skull bone are disrupted allowing brain pulsation to get transmitted) secondaries in the skull. Secondaries can also occur in long bones also.
Investigations
o Most often FNAC is inconclusive, because capsular and angioinvasion, which are the main features in follicular carcinoma, cannot be detected by FNAC.
o Frozen section biopsy was said to be useful earlier; but it is questionable now. In 15% cases frozen section biopsy may be inconclusive or facility for frozen section biopsy may not be available in many places, then initial hemithyroidectomy is done.
o Ultrasound abdomen, chest X-ray, X-ray bones are the other investigations required, CT head, body scan.
o Trucut biopsy gives tissue diagnosis, but danger of haem- orrhage and injury to vital structures like trachea, recur- rent laryngeal nerve, vessels are likely. It may be useful in lymphoma and anaplastic carcinoma; but it is not very well accepted.
Treatment
o Total thyroidectomy is done along with central node compart- ment dissection (level VI).
o Lateral cervical/neck node dissection (LCND) levels IIA, Ill, IV and VB) or MRND (with preservation of sternocleidomastoid, IJV, spinal accessory nerve) is done depending on involve- ment of one side or both (if node positive on imaging or FNAC only as therapeutic).
o Postoperativeradioactiveiodine(1131) therapywithadose of 100 mCi (3700 MBq) . Patient should be kept in isolation; excreta disposal and vomitus, blood, saliva should be in separate leak proof thrash bags.
o Maintenance dose of L-thyroxine 0.1 mg OD or T3 80 μg/ day is given lifelong. Immediate thyroxin supplementation is often not started following surgery to keep TSH level raised so that all extrathyroidal tissues that take up iodine will also take up radioiodine to achieve optimum radioablation. TSH level should be more than 30 mlU/L for this.
o
o on table frozen section biopsy is useful in negative FNAC but doubtful cases. Definitive procedure is undertaken once frozen section report comes on table. But in frozen section biopsy itself, 15% of follicular carcinoma report may be inconclusive or negative which causes difficulty in taking deci sion. In such occasion, hemithyroidectomy is done and once histology report of follicular carcinoma is obtained completion thyroidectomy is done usually immediately within a week. If biopsy report is delayed, then completion thyroidectomy is done after 6- 12 weeks.
Follow-up
o It is by radioisotope 1 123 scan done at regular intervals (6 months to one year) to look for secondaries.
o Thyroglobulin estimation is a good follo w-up method to decide for radioisotope study. Normal value (3-40 ng/mL). TG >50 ng/mL is abnormal. It should be done once in 3-6 months. Its raise signifies recurrent/metastatic disease. Serum thyroglobulin level estimation is of no value in preoperative assessment. After thyroidectomy thyroglobulin secretion is stopped, hence its level should not be traceable after total thyroidectomy.
o Ultrasound neck or MRI neck to identify early relapse. MRI neck is better.
Further Treatment
o If secondaries are detected therapeutic dose Ra 131 is given orally. L-thyroxine has to be stopped 6 weeks prior to RT, then required dose of Ra 131 is given (50-150 m curie).
o Radio remnant ablation (RRA)
• Initially thyroid radioisotope scan is done. If patient is on 300 μg suppressive dose of L-thyroxine, it should be stopped for 3-6 weeks so as to achieve serum TSH level above 30 M IU/I or two intramuscular injections of 0.9 mg of recombinant human TSH is given.
• If iodine isotope scan detects remnant disease, then 30-100 mCi of radio-ablation dose of 131 is given orally.RT will destroy occult microscopic disease. Post-ablation isotope scanning is done in 8 days. Later in intermediate and high risk patients, follow up body scan is done once in 6 months. Serum thyroglobulin estimation is done for 6-12 months, later once in 6 months; neck US at 6, 12 months and annually for 5 years. Raise in thyrog·lobulin level indicates for further whole body isotope scan. To detect metastases radioisotope I131 100- 200 mCi is given and 250-300 mCi is given for bone.
• Prior to radioactive iodine therapy following precautions should be taken-low iodine diet for 10 days; isolation when dose is more than 30 mCi; increase intake of oral fluid to maintain high urine output to avoid radioiodine induced bladder injury; sucking of lemon to avoid sialad- enitis; laxatives; reduced sperm count for 6-8 months; pregnancy should be avoided for 6- 12 months.
o Secondaries in bone are treated by external radiotherapy. Internal fixation should be done whenever there is patho- logical fracture.
o There is no role of chemotherapy for follicular carcinoma thyroid.
Resource : SRB's Manual of surgery ,6th edition